What is Tuberculosis?
The Philippines has the fourth largest number of TB cases in the world, according to the World Health Organization. In 2019, it was estimated that there were 599,000 people in the country who were infected with TB.
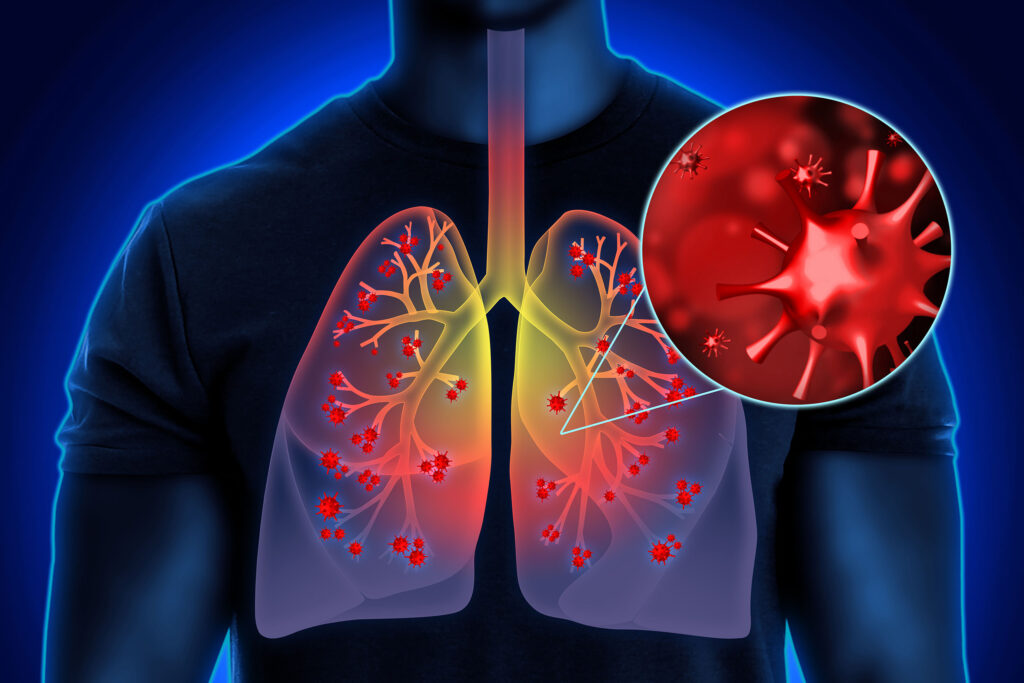
Tuberculosis (TB) is an airborne infectious disease that primarily infects the lungs. It can also affect the spine, hips, lymph nodes, and any other part of the body.

About one-quarter of the world’s population is infected by TB bacteria, but only 5% to 15% become sick with active TB disease. As a result, two TB-related conditions exist: latent TB infection (LTBI) and active TB disease. If not treated properly, both kinds of TB can be fatal.

Latent TB Infection (LTBI)
Latent TB infection (LTBI) occurs when a person is infected by TB bacteria that stays inactive in the body. People with LTBI do not show any symptoms and cannot spread TB to others. LTBI can be detected through a TB skin or blood test.
Active Tuberculosis Disease (Active TB)
If the immune system of a person with LTBI weakens, this could cause TB bacteria to grow and result in active TB disease. People with weak immune systems, such as those with HIV or cancer, are more at risk of developing active TB.
Symptoms
• Cough
• Fever
• Weight loss
• Night sweats
The cardinal, or main, signs and symptoms of TB last up to two weeks or more. People with active TB show these symptoms and may spread TB to other people.
Symptoms are often mild for many months. This may cause the patient with active TB to delay treatment and to infect more people without knowing.
If you or anyone you know is experiencing any TB symptoms, contact PTSI now.

Causes
TB is caused by bacteria called Mycobacterium tuberculosis or the tubercle bacilli. Like the common cold, TB is spread through droplets from an infected person with active TB when they cough, sneeze, talk, or sing.
It is NOT spread through:
• Insects, water, or blood
• Shaking someone’s hand
• Sharing food or drink
• Touching bed linens, clothes, or toilet seats
• Sharing toothbrushes
• Kissing
People at high risk of TB include:
• People living with HIV (PLHIV)
• People with weakened immune systems
• People with history of previous TB treatment
• Elderly
• Diabetics
• Smokers
• Close contacts of TB patients
• Healthcare workers
Treatment
Only 43% of TB cases in the Philippines were detected by health systems in 2020. At present, there are approximately 342,000 TB cases missing from the country’s records.
TB can be cured and prevented. Early detection is key. When left untreated, TB could be fatal.


PTSI adheres to the National TB Control Program Manual of Procedures in the screening, diagnosis, and treatment of all its patients.
Screening
Case finding is the identification of presumptive TB by symptoms-based screening, chest x-ray or both. Presumptive TB can be identified through systematic screening in health facilities or among targeted populations in crowded places, the community, or workplaces.
Diagnosis
Once a presumptive TB case is identified, the patient must be tested to confirm the presence of TB bacteria in the body.
PTSI primarily performs chest x-rays and sputum tests. A patient may be diagnosed with TB if their chest x-ray findings are strongly suggestive of TB or they have a positive sputum test.

Chest X-ray
• Detects abnormalities in the lungs that may be compatible with TB

Xpert MTB/RIF sputum test
• The primary diagnostic test for TB in adults and children
• Also detects multidrug-resistant TB (MDR-TB)
Other Tests
Mantoux tuberculin skin test (TST)
• A skin reaction test that uses tuberculin to detect TB
• Recommended for children under 5 years old
Interferon-gamma release assays (IGRAs blood tests)
• A blood test for detecting TB
• Recommended for people who have received the TB vaccine or Calmette (BCG), or for people who cannot return for a second TST appointment

Treatment
TB can be cured completely by taking the prescribed medicine and attending check-ups for at least 6 months. This treatment is called the Directly-Observed Treatment, Short-Course (DOTS), or Tutok-Gamutan.
DOTS is approved by the World Health Organization and is available in all Southeast Asian countries.
People with pulmonary TB, or TB of the lungs, should stay home from work or school to avoid spreading it. They may stop being infectious after taking the prescribed TB drugs for 2 weeks. However, they must still follow the rest of the prescribed treatment period afterwards.
The DOTS regimen consists of an intensive phase of 2 months, followed by a continuation phase of 4 months.
Duration of different TB treatments
• 6 months - Drug-susceptible TB (TB DOTS)
• 9–20 months - Multidrug-resistant TB (MDR-TB treatment)
• 12 months - Severe drug-susceptible extrapulmonary TB (ETB treatment)
If a patient stops taking their medicine before the treatment period ends, the TB bacteria in their body can become stronger and more resistant to drugs. This may lead to MDR-TB, which is harder to treat.